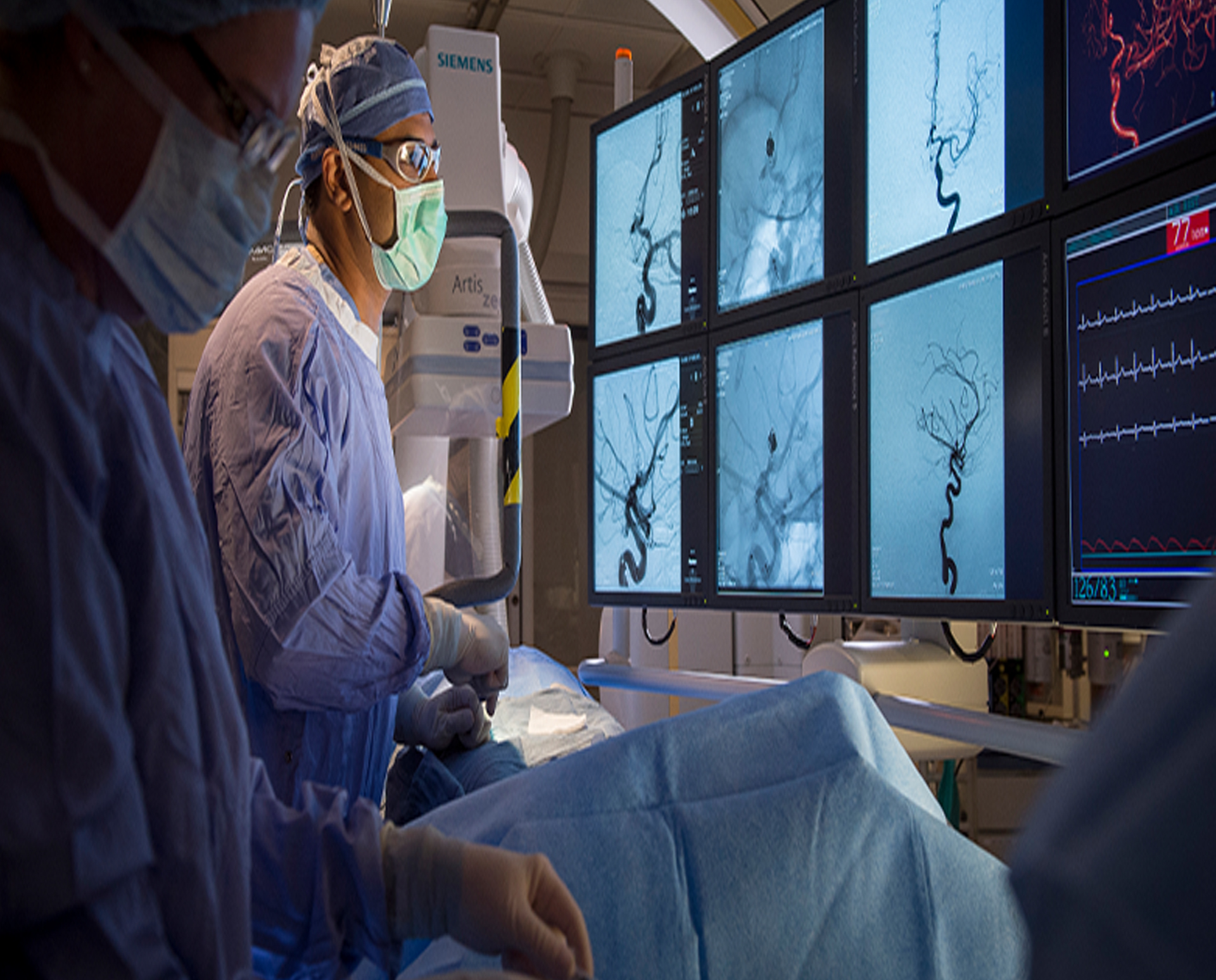
Interventional radiology (IR) is a fascinating and rapidly evolving specialty in medicine that utilizes minimally invasive techniques to diagnose and treat various medical conditions. By harnessing advanced imaging technologies—such as X-rays, CT scans, and ultrasounds—interventional radiologists can precisely guide instruments through the body, eliminating the need for large surgical incisions. This blog delves into the intricacies of interventional radiology, highlighting its numerous benefits and outlining some common procedures.
What is Interventional Radiology?
Interventional radiology bridges the gap between imaging and therapeutic intervention. It combines sophisticated imaging modalities with minimally invasive techniques, enabling healthcare providers to diagnose and treat diseases without resorting to traditional surgical methods. Unlike conventional surgery, which often necessitates extensive incisions and longer recovery times, IR procedures typically involve smaller incisions or even no incisions at all, significantly reducing trauma to the body. This innovative approach not only minimizes discomfort but also facilitates faster recovery, allowing patients to return to their daily lives with less interruption.
Key Areas of Practice
Interventional radiologists are trained to perform a diverse array of procedures across various medical specialties. Here are some prominent areas of practice:
Vascular Interventions: Interventional radiologists address conditions affecting blood vessels, such as performing stenting to alleviate blockages in arteries or using embolization techniques to control bleeding from trauma or tumors. These procedures enhance blood flow and mitigate the risks associated with vascular diseases.
Oncological Interventions: In the fight against cancer, interventional radiology plays a pivotal role. Techniques like radiofrequency ablation (RFA) employ heat to destroy cancerous cells, while transarterial chemoembolization (TACE) delivers chemotherapy directly to tumors, maximizing efficacy while minimizing systemic exposure.
Gastrostomy and Drainage Procedures: Interventional radiologists perform essential procedures such as placing feeding tubes for patients who cannot eat by mouth or draining abscesses and fluid collections. These interventions are critical for managing complications related to various gastrointestinal disorders.
Biopsy Procedures: With the help of imaging guidance, interventional radiologists can perform biopsies with remarkable accuracy. By using thin needles, they obtain tissue samples from suspicious areas, aiding in the diagnosis of cancers and other diseases.
Benefits of Interventional Radiology
The advantages of interventional radiology are manifold:
Minimally Invasive: The small incisions or non-invasive access points used in IR result in less pain and scarring, significantly enhancing patient comfort and satisfaction. Patients often report a more positive experience compared to traditional surgical approaches.
Reduced Recovery Time: Many IR procedures can be performed on an outpatient basis, allowing patients to return home the same day. This swift turnaround is particularly beneficial for individuals who wish to minimize time away from work or family.
Lower Risk of Complications: The minimally invasive nature of IR reduces the likelihood of complications such as infections, prolonged hospital stays, and the need for extensive rehabilitation.
Real-Time Imaging Guidance: Advanced imaging technologies provide real-time visualization, allowing interventional radiologists to accurately navigate instruments within the body. This precision enhances the effectiveness of procedures and improves overall patient outcomes.

Common Interventional Radiology Procedures
Angioplasty and Stenting: This procedure is crucial for patients with cardiovascular disease. Angioplasty involves using a balloon to open narrowed arteries, while stenting places a small mesh tube to keep the artery open, enhancing blood flow and reducing the risk of heart attacks.
Embolization: A versatile procedure, embolization can be used to block abnormal blood vessels supplying tumors, manage uterine fibroids, or control bleeding from traumatic injuries. By selectively blocking blood flow, interventional radiologists can effectively treat various conditions.
Biliary Interventions: In cases where bile ducts become obstructed due to tumors or gallstones, interventional radiologists can perform procedures to relieve the blockage. This may involve placing stents to keep the ducts open and restore proper bile flow, alleviating pain and preventing complications.
Peripherally Inserted Central Catheter (PICC): PICC lines provide long-term access for patients needing frequent intravenous treatments, such as chemotherapy or antibiotics. This procedure minimizes discomfort compared to repeated needle sticks, enhancing patient quality of life.
Vertebroplasty and Kyphoplasty: These procedures address vertebral compression fractures, often resulting from osteoporosis. By injecting bone cement into the fractured vertebrae, these interventions stabilize the spine, relieve pain, and improve mobility.
The Future of Interventional Radiology
As technology advances, the landscape of interventional radiology continues to evolve. Innovations such as robotic-assisted procedures enhance precision and control, while improved imaging techniques lead to better outcomes. Additionally, the integration of artificial intelligence in diagnostics and treatment planning promises to further refine interventional strategies, allowing for even more personalized and effective patient care.

